The original article appeared on AARP’s blog on August 13, 2020
The COVID-19 pandemic is disproportionately impacting Native Americans, magnifying a long-standing history of structural and economic inequality that results in health disparities. The full extent of that impact, however, is unknown due to a dearth of data on the race and ethnicity of U.S. citizens tested for, infected with, and dying from COVID-19. Nevertheless, the data reveal trends that are startling, highlighting the need for both better data and policy action.
Health Disparities A Result of Longstanding Inequality
As with certain other groups including African Americans and Hispanics, the coronavirus presents a substantial risk for Native Americans, especially older adults, due to the high prevalence of underlying health conditions in this group. Compared to all other racial groups, American Indians and Alaska Natives have the highest mortality rates from multiple chronic conditions, including heart disease, stroke, liver disease, kidney disease, lower respiratory disease, and diabetes. They also report the lowest self-rated health status and have the shortest life expectancy of any racial or ethnic group.
These health disparities are a result of deep-rooted structural inequality caused by government policies in existence for centuries. American Indian and Alaska Native communities often lack access to adequate health care, safe housing, clean water, and reliable transportation, and many hospitals serving Native Americans are understaffed. These long-standing disparities result in Native Americans being particularly vulnerable to COVID-19.
Initial Data Show Heavy Toll of COVID-19 on Native Americans, but Data are Lacking
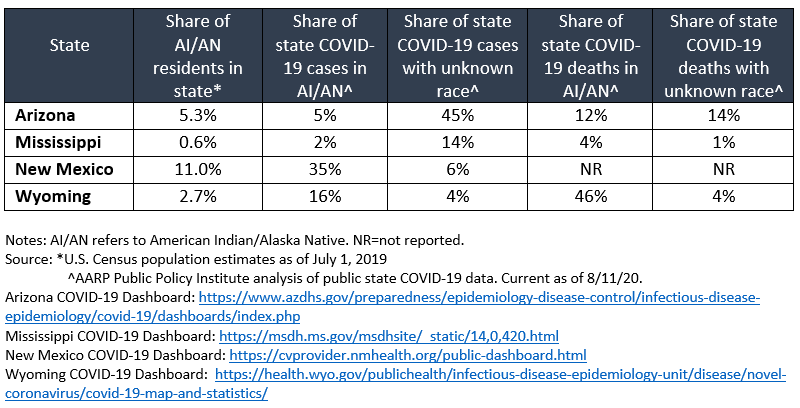
Preliminary data show COVID-19 is having a devastating impact on Native Americans. According to the Centers for Disease Control and Prevention (CDC), the COVID-19 hospitalization rate is five times higher for American Indians and Alaska Natives than for whites. COVID-19 cases and deaths for American Indians and Alaska Natives in Wyoming, Arizona, New Mexico, and Mississippi are higher than would be expected based on their share of the state population (table). In Wyoming, for example, American Indians and Alaska Natives make up 2.7 percent of the population but represent 16 percent and 46 percent of COVID-19 cases and deaths in the state, respectively. Moreover, Native Americans are more likely than any other racial group to have their race misclassified on death certificates. The high proportion of COVID-19 cases and deaths with unknown race suggests the burden among Native Americans may be even higher than reported.
As is the case for all racial and ethnic groups, the true scope of the problem is unknown. As of August 11, approximately 5 million Americans have been infected with the coronavirus, yet the CDC does not report race and ethnicity for more than half of those cases. Furthermore, while all states except North Dakota capture at least some race and ethnicity data for COVID-19 cases, nearly half the states (47%) do not include American Indian/Alaska Native as a racial category in their reports. Moreover, of the six states with the highest share of Native American residents—Alaska (15.6%), New Mexico (11%), South Dakota (9.4%), Oklahoma (9%), Montana (6.7%), and North Dakota (5.6%)—only two (Alaska and Oklahoma) report COVID-19 deaths by race and ethnicity.
A Necessary First Step: Comprehensive Racial and Ethnic Data
Because American Indians and Alaska Natives have disproportionately high rates of diseases that are known risk factors for serious complications from COVID-19, it is imperative that we know the full impact of the coronavirus in Native American communities.
At a minimum, demographic data—including race (and tribal affiliation if applicable), ethnicity, and age—must be collected for every person tested for the coronavirus, as well as for COVID-19 cases, hospitalizations, and deaths. State public health departments should regularly analyze and publicly report these disaggregated data. Currently, only six states (Delaware, Illinois, Indiana, Kansas, Nevada, and Utah) report COVID-19 testing data by race and ethnicity.
Resources must be made available for areas and communities facing the highest risk of COVID-19 to ensure they can effectively respond to the pandemic, starting with effective data collection. The Coronavirus Aid, Relief, and Economic Security (CARES) Act directed $8 billion in funds to tribal communities and their government-owned enterprises, but they have only received $4 billion to date. The CARES Act also allotted an additional $2 billion for federal programs that serve Native American communities, including $1 billion for the Indian Health Service, an amount not nearly high enough for a system the U.S. Commission on Civil Rights reports is already underfunded by $32 billion.
Longer-term, policy makers must do more to address the long-standing health disparities impacting Native American communities, including ensuring sufficient funding and resources for tribal health. They must also invest in the social determinants of health—the conditions in the places where people live, learn, work, and play that impact health—which contribute to these disparities. This includes tackling racism and improving access to affordable housing, reliable transportation, and good paying jobs, to name a few.
AUTHORS Elizabeth A. Carter, Olivia Dean, Michael E. Bird
